Gene therapy for heart failure: how does gene therapy work?
Gene therapy introduces a genetic material (DNA) into the cells to make a beneficial protein. In heart disease, gene therapy may be able to place a normal copy of the gene into the human cell to change how the cell works with the end goal of correcting the disease. To insert the gene into a cell, gene therapy uses a vector or carrier to introduce the gene into the human cell.
Non viral vectors are relatively easy to produce and consist of plasmid (DNA that can reproduce). The vector lets the gene take a piggyback ride on it to reach the diseased cells. Once there, it is absorbed into the cells to help stimulate the body to make more beneficial protein. They are delivered by direct administration, as in this example of the patient treated in the STOP-HF JUVENTAS trial.
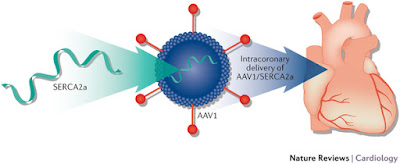
In this case, stroma cell-derived Factor-1 (SDF-1) was injected at multiple sites inside the left ventricle. By avoiding exposure to blood it prevents some weakening of the vector and does not affect other organs as much. Viral vectors or carriers have become the preferred method of delivery of gene therapy because of their high efficiency and capability. The adeno-associated virus (AAV) has emerged as the preferred factor because it is safe and can have a long term effect. This AAV virus is not known to cause disease in humans. Delivery of genetic material through the circulation can be accomplished either by direct injection through the coronaries. It can also be injected through bypass graft to the coronaries or a retrograde infusion through the coronary sinus into the venous system of the heart.
Gene therapy targeting calcium regulating protein:
Heart failure is characterized by multiple defects in handling the calcium involved in excitation and contraction of the heart cells. Abnormal adjustment of calcium inside the cell can be attributed in part to decreased activity of an enzyme called SERCA2a. In heart failure, there are lower levels of this enzyme in heart muscle cells which makes the heart not contract as much as it should. . Increasing the enzyme in the heart muscle cells of animals with heart failure improves heart function. Preliminary data showed that intracoronary infusion of (AAV1) adeno-associated virus delivering the gene of this enzyme to the heart improved symptoms, functional status and LV function in patients with advanced heart failure.
CUPID phase 2b trial was a multicenter, double-blind, placebo control, randomized study of AAV1/SERCA2a (attenuated virus and the gene) in patients with advanced heart failure. Patients ages 18-80 with stable class 2-4 heart failure with ischemic or nonischemic cardiomyopathy were enrolled. The following images depict the coronary angiogram of one of our patient at CardiologyPC. He is a 59-year-old patient who underwent bypass surgery 12 years prior and a biV-ICD 3 years prior to enrollment. The patients was hospitalized 5 months before his enrollment in CUPID because of heart failure decompensation.